- Author: Kathy Keatley Garvey



Now, newly published research on ovarian cancer, involving an anti-inflammatory compound discovered and developed in the Bruce Hammock lab at the University of California, Davis, and tested at Harvard Medical School on mice models, indicates that the compound not only suppresses inflammation but reduces cancer growth, acting as a “surge protector.”
“We are excited about this research and its potential,” said Hammock, a UC Davis distinguished professor who holds a joint appointment with the Department of Entomology and Nematology and the UC Davis Comprehensive Cancer Center. “Chemotherapy and surgery, the mainstays of conventional cancer treatment, can act as double-edged swords. It is tragic that the very treatments used to cure cancer are helping it to survive and grow.”
The research is a “novel approach to suppressing therapy-induced tumor growth and recurrence,” said the 13-member team from Harvard Medical School/Beth Israel Deaconess Medical Center (BIDMC), UC Davis, Institute of Systems Biology of Seattle, and Emory University School of Medicine of Atlanta.
Their paper, “Suppression of Chemotherapy-induced Cytokine/Lipid Mediator Surge and Ovarian Cancer by a Dual Cox-2, sEH Inhibitor,” appears today in the Proceedings of the National Academy of Sciences (PNAS).
“To prevent tumor-recurrence after therapy, it will be critical to neutralize the inherent tumor-promoting activity of therapy-generated debris,” said lead author Allison Gartung of Harvard Medical School/BIDMC. “Our results indicate that a dual COX-2/sEH inhibitor may offer a novel alternative to protect the body from a debris-mediated inflammatory response.”
Gartung said that the study confirmed that chemotherapy-killed ovarian cancer cells “induce surrounding immune cells called macrophages to release a surge of cytokines and lipid mediators that create an optimal environment for tumors to survive and grow.”
The team treated the mice models with a dual lipid pathway inhibitor discovered several years ago in the Hammock lab. It integrates two anti-inflammatory drugs (COX-2 inhibitor and soluble expoxide hydrolase (sEH) inhibitor) into a single molecule with the aim of reducing tumor angiogenesis and metastasis.
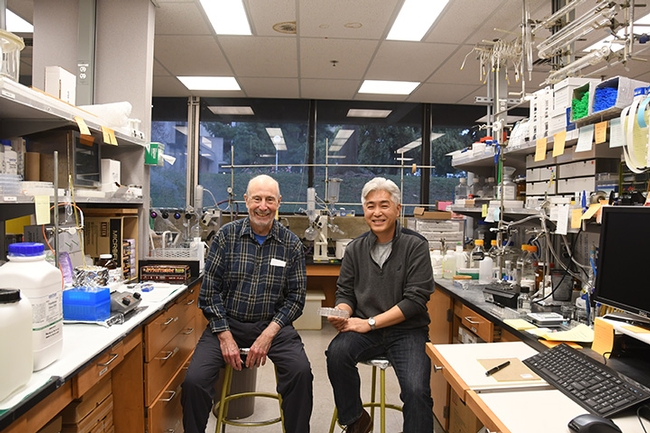
Chemist Sung Hee Hwang of the Hammock lab developed the compound, known as PTUPB, for the study. “The dual inhibitor here follows earlier work we did with it, blocking breast and lung tumors in mice,” Hammock said. “PTUPB is already being clinically evaluated for its therapeutic properties in other diseases.” Chemist Jun Yang of the Hammock lab did the mass spectrometry, showing how stabilization of lipid mediators reduces cancer growth and metastasis.
Lead researcher Dipak Panigrahy, a former Harvard physician turned full-time researcher, described chemotherapy and surgery “as our best tools for front-line cancer therapy, but chemotherapy and surgery create cell debris that can stimulate inflammation, angiogenesis, and metastasis. Thus, the very treatment used by oncologists to try to cure cancer is also helping it survive and grow. Overcoming the dilemma of debris-induced tumor progression is critical if we are to prevent tumor recurrence of treatment-resistance tumors which lead to cancer therapy failure.”
The tumor cell debris generates a “cytokine surge” that can result in a perfect storm for cancer progression. “The dual inhibitor acts as a surge protector,” Panigrahy said.
Panigrahy, who led angiogenesis and cancer animal modeling in the laboratory of Judah Folkman, a leading cancer research laboratory, based the debris model on his mother's chemotherapy treatments, and dedicated the research to his mother and “all other women who lost their lives to ovarian cancer.” American Cancer Society statistics show that among women, ovarian cancer ranks fifth in cancer deaths. A woman's risk of ovarian cancer is about 1 in 78; every year more than 14,000 die from the disease.
“Traditional cancer therapy sets up a dilemma,” Panigrahy commented. “Yes, we need to kill cancer cells but the inevitable byproduct of successfully doing so also stimulates tumor regrowth and progression. The more tumor cells you kill, the more inflammation you create, which can inadvertently stimulate the growth of surviving tumor cells. Overcoming the dilemma of debris-induced tumor progression is paramount if we are to prevent tumor recurrence of treatment-resistant tumors – the major reason for failure of cancer therapy. Our studies potentially pave the path for a new strategy for the prevention and treatment of chemotherapy-induced resistance with potential to translate to the clinic. If successful, this approach may also allow us to reduce the toxic activity of current treatment regimens.”
“The collaborative work in this paper not only defines a common problem with current cancer therapy, but it actually offers a potential solution to reduce metastasis and tumor growth following therapy,” said Primo Lara Jr., director of the UC Davis Comprehensive Cancer Center and associate director of Translational Research. “I am pleased that our Center was involved in this exciting project and we hope we can be involved in translating this basic research to the clinic.”
Panigrahy said that non-steroidal anti-inflammatory drugs (NSAIDs), which include aspirin and ibuprofen, reduce pain, fever and inflammation “bit may have severe side effects including stomach and brain bleeding as well as severe cardiovascular and kidney toxicity. They also do not specifically enhance clearing of debris.”
“We are exploring all options to translate PTUPB to cancer patients especially in combination with current cancer therapies such as chemotherapy, radiation, immunotherapy, or surgery which either directly or indirectly may generate tumor cell debris,” Panigrahy said. “Our next step is to investigate whether our findings are consistent with clinical studies involving human cancer.”
The Hammock lab has been researching the sEH inhibitor for 50 years. As a graduate student at UC Berkeley, Hammock co-discovered the sEH inhibitor with fellow graduate student Sarjeet Gill, now a distinguished professor at UC Riverside.
"We have a series of papers largely in PNAS, with the Panigrahy group showing first our soluble epoxide hydrolase inhibitors block tumor growth and metastasis when used with omega3 fish oils or with COX inhibitors and the role for these compounds in regulating a number of mediators of cancer growth," Hammock said.
Multiple grants funded the research. Hammock, the 31-year director of the UC Davis Superfund Program, received funds the National Cancer Institute and the National Institute on Environmental Health Sciences. The Panigrahy laboratory is funded by the Credit Union Kids at Heart Team. Other grants came from the C. J. Buckley Pediatric Brain Tumor Fund, Molly's Magic Wand for Pediatric Brain Tumors, the Markoff Foundation Art-in-Giving Foundation, the Kamen Foundation, Jared Branfman Sunflowers for Life, and the Joe Andruzzi Foundation. An NIH T32-training grant funded Gartung's work.
The Team
Allison Gartung completed her doctorate at Wayne State University in 2016 and has since served as a postdoctoral research fellow at Harvard Medical School/BIDMC. Highly honored for her work, she won the highest award for a post-doctoral fellow (Santosh Nigam Award) at the 15th International Conference on Bioactive Lipids in Cancer, Inflammation and Related Diseases, held in 2017 in Puerta Vallarta, Mexico. She served as a guest editor of a special double-issue of 24 invited world-experts in Cancer and Metastasis Reviews on Bioactive Lipids.
Dipak Panigrahy was accepted into medical school at Boston University at age 17. He trained in surgery with Dr. Roger Jenkins, who performed the first liver transplant in New England. Over the past decade, Panigrahy led angiogenesis and cancer animal modeling in the Judah Folkman laboratory. He joined the Beth Israel Deaconess Medical Center in 2013, and in 2014 was appointed assistant professor of pathology, and currently has a laboratory in the Center for Vascular Biology Research. Panigrahy is the expert on the team for preclinical tumor models and examining novel concepts for cancer therapy at the preclinical stage –the diversity of models he has created and worked with is unmatched.
Bruce Hammock, UC Davis distinguished professor, is the world expert and discoverer of the dual COX2-sEH inhibitor. He received his doctorate in entomology/toxicology from UC Berkeley and joined the UC Davis faculty in 1980. Highly honored by his peers, Hammock is a fellow of the National Academy of Inventors, which honors academic invention and encourages translations of inventions to benefit society. He is a member of the U.S. National Academy of Sciences, and the recipient of scores of awards, including the Bernard B. Brodie Award in Drug Metabolism, sponsored by the America Society for Pharmacology and Experimental Therapeutics; and the first McGiff Memorial Awardee in Lipid Biochemistry,
Mark Kieran of Bristol-Myers Squibb and Professor Vikas Sukhatme (Dean of Emory School of Medicine), both senior co-authors, are leading world-experts on personalized medicine approaches to support the treatment of cancer patients. Kieran is a leading oncologist with expertise in translating novel therapeutic modalities (beyond chemotherapy/irradiation) into the clinic. Plans for clinical trials involving PTUPB are underway.
Professor Sui Huang, with the Institute for Systems Biology (ISB), is known as the world's leading expert on systems biology and debris-induced tumor growth.