Posts Tagged: Gail Woodward-Lopez
Online ordering for fast food inconsistent with healthy beverage law, study finds
Lack of specific language for online context makes assessing compliance difficult
Beverages offered on fast-food restaurant websites and platforms such as DoorDash, GrubHub and UberEats often do not adhere to the spirit of California's healthy beverage law for children's meals, according to a new study from University of California researchers.
California's healthy-by-default beverage law (SB1192), which went into effect at the beginning of 2019, requires restaurants to offer only plain or sparkling water with no added sweeteners, unflavored milk, or unflavored non-dairy milk as the default beverage in “kids meals.” The law also requires that menus, menu boards and advertisements for those meals include only approved default options.
The law was passed to address increasing rates of childhood obesity and related chronic diseases, with sugary beverages factoring as a significant contributor to those poor health outcomes.
“Healthy-by-default beverage laws work by making the healthiest choice, the easiest choice for families,” said the study's lead author, Hannah Thompson, senior epidemiologist for the UC Nutrition Policy Institute and assistant adjunct professor at the UC Berkeley School of Public Health. “Drinking sugar-sweetened beverages like sodas has been directly linked to health problems such as Type II diabetes, heart disease and cavities.”
Researchers at the NPI – a program of UC Agriculture and Natural Resources – found that most fast-food restaurants serving low-income census tracts did not offer beverages online in a way that is consistent with SB1192. The study focused on those neighborhoods because children from low-income families consume sugar-sweetened beverages in greater quantities, likely exacerbating health disparities.
Published online in the journal Public Health Nutrition, the study looked at a random sample of 254 “quick service restaurant” sites and collected observations from their restaurant-specific websites and three of the most popular online platforms that deliver their menu items – DoorDash, GrubHub and UberEats.
Researchers developed four increasingly restrictive criteria – incorporating beverage availability, upcharges and presentation of beverage options – to assess the implementation of SB1192 in these online ordering contexts. Half of their observations met their most lenient criteria, while less than 6% were consistent with their most restrictive – findings that Thompson called “discouraging.”
“It means families have to work harder to make the healthiest drink choices for their children,” she said. “This also means the law is likely not nearly as successful as it could be in its intent to help reduce sugary drink consumption by kids.”
The researchers had to create their own criteria for “compliance” with the law because, as written, SB1192 does not specifically mention online ordering, which has become increasingly popular due to the COVID-19 pandemic.
“Part of what makes it hard in the online context is that the law was written using language very specific to the in-restaurant physical space, making interpretation of compliance with the law for meals sold online challenging,” Thompson explained. “I'd love to see amended language in the law specific to meals sold online.”
Thompson also said she would like to see “clear and effective” communication with fast food restaurants and online delivery platforms so that they fully understand the healthy beverage law – as well as the use of a monitoring system that could help ensure compliance.
“Laws, which target system-level changes, are one of the most important public health tools we have to reduce sugary drink consumption and improve health for youth of all backgrounds,” she said. “But laws are only as strong as the structures in place to ensure their successful implementation.”
The other NPI-affiliated authors of the study are Senior Evaluators Anna Martin and Ron Strochlic, Evaluation Associate Sonali Singh, and Associate Director of Research Gail Woodward-Lopez, the principal investigator.
New policies can inspire families to provide healthy beverages to children
At fast food and sit-down restaurants across California, kids' meals come with water or milk automatically. At least, that should be the case since state law requires restaurants to offer the healthy beverages by default to reduce the amount of sugary beverages served to children.
California Senate Bill 1192, authored by Sen. Bill Monning (D-San Luis Obispo), went into effect Jan. 6, 2019, but research by the UC Nutrition Policy Institute (NPI) has found that implementation has not been universal and more can be done. The results, along with results from a similar study in Wilmington, Del., were published Aug. 20 on HealthyEatingResearch.org.
Before the law, 10% of menu boards observed by the researchers in California listed only the healthy beverages. Data collected after the law went into effect showed 66% of menu boards list the healthy default beverages. The researchers also collected data on the proportion of cashiers who verbally offered only healthy beverages with kids' meals when orders were placed. This happened only 5% of the time before the law was enacted, and dropped to 1% after.
“Parents look at menu boards and kids look at menu boards, but it is likely that what the cashier says also influences which drink they choose,” said Lorrene Ritchie, NPI director and UC Cooperative Extension nutrition specialist. Ritchie was the lead researcher on the California portion of the study. “In our data collection, we would order a kids' meal and wait for them to offer a drink. But mostly they said, ‘What drink do you want?' instead of ‘Do you want water or milk with that?'”
The law doesn't specify whether the cashier must offer the default beverages, but the spirit of the law suggests they should, as it would likely have a greater impact on the selections that children and parents make, Ritchie said.
According to Gail Woodward-Lopez, an NPI researcher and co-investigator on the study, most restaurant managers expressed support for the legislation, but didn't know much about it.
“NPI in partnership with the California Department of Public Health is working with some local health departments to provide training and materials to help restaurants comply with the letter and spirit of the law,” Woodward-Lopez said. “Our next step is to measure whether this health department support is effective.”
The dire need to direct children away from sugary sodas is clear. Empty calories from soda and other sugar-sweetened beverages is the No. 1 cause of obesity in children, Ritchie said. Obese children are at least twice as likely as non-obese children to become obese adults. Obese children and adults are at greater risk for Type 2 diabetes, heart disease, stroke, high blood pressure, high cholesterol, certain cancers, asthma, low self-esteem, depression and other diseases. The Centers for Disease Control and Prevention names obesity as one of the conditions that increase risk of severe illness from COVID-19.
Many open questions remain, such as how drinks are portrayed on drive-thru signs and offered by drive-thru order takers. The COVID-19 pandemic has also altered the way Americans purchase food, with increased online ordering, delivery and drive-thru usage. In-store kiosk ordering is also growing in popularity.
“The role of default beverage policies in this context is important and not well understood,” Woodward-Lopez said.
Woodward-Lopez and Ritchie are working with colleagues around California and across the country to design follow-up studies of newer food technologies and beverage policies being passed elsewhere, to determine how government policies can protect children's health by steering them toward healthy beverage consumption.
The newly published research was funded by the Robert Wood Johnson Foundation and by the California Department of Public Health with funding from the United States Department of Agriculture.
Children are getting healthier, but the obesity crisis is not over
Real progress has been made in tackling the epidemic of childhood obesity since the first California Childhood Obesity Conference was held 20 years ago, but there is more work to be done.
“Collectively, we have come so far,” UC Nutrition Policy Institute Director Lorrene Ritchie told an audience of 1,025 public health, nutrition education, research, and other professionals at the event in Anaheim in July 2019. NPI was one of six conference hosts.
In the last 20 years:
- Federal school meal standards have been revised so that the food children eat at school is healthier than the lunches they bring from home.
- Sugar-sweetened beverages are no longer available to students during the school day.
- Foods provided by the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) are healthier and give mothers incentive to breast feed their babies.
- The Supplemental Nutrition Assistance Program (SNAP) education component is now linked to policy, systems and environmental changes.
- The Child and Adult Care Food Program now provides healthier meals and snacks to children in childcare centers and homes across the country.
The average quality of the diet of American children has improved, but the rate of childhood obesity in the United States is still too high.
According to the Centers for Disease Control and Prevention, 18.5% of U.S. children and adolescents 2 to 19 years old are obese – about 13.7 million youth in all. The rates trend higher in minority communities, with 25.8% of Latinx youth and 22% of African American youth obese. Obesity is also more prevalent among children in families with low incomes.
Obesity, which is defined in children as a body mass index at or above the 95th percentile of CDC growth charts, is associated with poorer mental health status, reduced quality of life, and increased prevalence of diabetes, heart disease, stroke and some types of cancer.

The vice president of UC Agriculture and Natural Resources, Glenda Humiston, pledged the organization's commitment to community health and wellbeing at the Childhood Obesity Conference. UC ANR is the umbrella organization of the Nutrition Policy Institute, UC CalFresh Healthy Living, UC Cooperative Extension, 4-H Youth Development, the UC Master Gardener Program and the California Naturalist Program, among others.
“Going forward, solutions to the obesity epidemic are multidisciplinary,” Humiston said. “NPI does world class work in conducting research to influence nutrition policy. We need to harness 4-H. Master Gardeners are increasingly focusing on edible gardens. CalNat is getting people out into nature. We are finding synergies in community wellness.”
Humiston has dedicated UC ANR resources to finding and implementing solutions to the obesity crisis.
“I'm looking forward to working with all of you – public and private organizations – to design a way to move forward,” she said.
The opening keynote presentation at the conference featured Patricia Crawford, NPI's Senior Director of Research emeritus, a pioneer in addressing the growing problem of childhood obesity during her long career. Beginning in the 1970s, she recognized that childhood obesity was on the rise and launched several studies to search for the causes and potential solutions.
In one study, Crawford followed a group of 9-year-old African American girls over a period of 10 years to determine why these youth were growing up heavier than other adolescents.
“Finally, we began to get some answers,” Crawford said. “We learned obesity wasn't the children's fault. They were living in environments that made the unhealthy choice cheaper and easier to find. It's so unfair for people who have fewer resources. Health disparities has to be the No. 1 thing we are working on to address chronic disease rates in this country.”
“The solution to obesity is prevention. It's cheaper and more effective than treatment,” Crawford continued. “Healthy food is a taste that is easy to acquire if it is not preempted by junk food.”
Crawford said she honed in on the best strategies for prevention by actively listening to people struggling to make healthy choices
“There is a chasm between research and community,” Crawford said. “We have to get people together from the research level and the policy level with folks on the ground. We need to learn from people.”
UC Berkeley nutritionist welcomes MyPlate
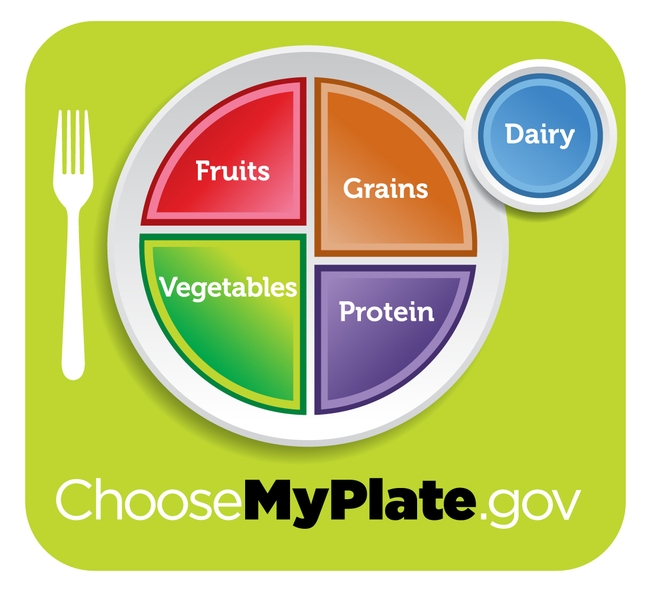 USDA introduced MyPlate yesterday. |
 MyPyramid served as the USDA's food guide icon from 2005 to 2011. |
The associate director of the UC Berkeley Center for Weight and Health, Gail Woodward-Lopez, said USDA's new food icon, MyPlate, is more in line with current nutrition science, according to The Bay Citizen.
"It has the potential to be more effective," Woodward-Lopez was quoted. "The pyramid involved counting the number of servings for the day. So when do you make that decision? When you go to bed at night?"
She said the plate in consistent with the Center's findings on obesity prevention for children and adults: "Lots of fruits and vegetables, less refined grains, don't overdo the protein."
Something interesting I've noticed about the news coverage of MyPlate - including the Bay Citizen story - is references to the pyramid it replaces. The original Food Guide Pyramid, introduced in 1992, was replaced by MyPyramid 2005. However, some journalists have ignored the six years of MyPyramid, declaring that MyPlate replaces the long-retired hierarchical Food Guide Pyramid.
See the CNN story (image below) for another example of this common misunderstanding.





