Calag Archive
Calag Archive
How can Californians be overweight and hungry?
Publication Information
California Agriculture 58(1):12-17. https://doi.org/10.3733/ca.v058n01p12
Published January 01, 2004
PDF | Citation | Permissions
Abstract
The United States is experiencing an epidemic of obesity in both adults and children, particularly among low-income populations. In fact, overweight has replaced malnutrition as the most prevalent nutritional problem among the poor. We examine this seemingly paradoxical relationship and explore the causes and consequences of overweight, obesity and food insecurity. In a UC Cooperative Extension Body Weight and Health Workgroup study of 561 low-income Latino mothers and their young children, we found important differences in the association between family food insecurity and overweight status for mothers and their children. Forty percent of the women were overweight and 37% obese, and 22% of their children were overweight. Furthermore, U.S.-born mothers who were food insecure as children were more likely to be obese adults. Awareness and understanding of the link between food insecurity and weight gain will facilitate the efforts of schools, food assistance programs, the food industry and others in the community to provide effective nutritional programs.
Full text
Obesity has become an epidemic among U.S. adults and children during the past 30 years and threatens to overwhelm our health care system. According to the 1999-00 National Health and Nutrition Examination Survey (Flegal 2002), 64% of U.S. adults (ages 20 to 74) are either overweight or obese. The percentage of overweight children and adolescents has tripled in the last 30 years (Ogden et al. 2002). An overweight child is likely to become an overweight adult, with consequent health risks. Approximately three-quarters of teenagers who are overweight will grow up to be overweight or obese adults (Whitaker et al. 1997).
Although overweight is often considered a problem of overeating rather than hunger and scarcity, low-income adults and children have gained the most weight in recent decades. Rates of obesity and overweight among the poor are increasing, while the number of poor Americans experiencing food insecurity remains high, at an estimated 30 million (Olson and Holben 2002). How can we explain the coexistence of overweight and food insecurity among the poor? To answer this question, UC Cooperative Extension (UCCE) advisors and specialists — members of the Body Weight and Health Workgroup — examined a large sample of low-income Latino mothers and their young children.
To explore the relationship between overweight and food security, a UC workgroup studied 561 low-income Latino mothers and their children. Forty percent of the women were overweight and 37% obese, and 22% of their children were overweight. UC Cooperative Extension nutrition instructor Mariana Castro measures Samuelito in Richmond.
Weight and health, economic status
Overweight is associated with increased risk of disease, causing considerable concern among health care professionals (). Numerous chronic diseases are associated with childhood as well as adult overweight. Diseases associated with obesity and overweight will soon rival cigarette smoking as the leading cause of preventable premature death and disability in the United States, according to the U.S. Surgeon General's Call to Action (US DHHS 2001).
The prevalence of obesity in the United States has grown rapidly in the last 30 years, during a time of economic prosperity. However, the increasing incidence of obesity does not necessarily reflect a more affluent lifestyle or increased availability of food resources. Socioeconomic status is one way to gauge family or household food-security status. Indeed, people of low socioeconomic status and those who experience food insecurity, along with certain racial and ethnic groups, are at a disproportionately higher risk for obesity and health-related conditions. In fact, overweight has replaced malnutrition as the most prevalent nutritional problem among the poor.
Evidence suggests that associations between socioeconomic status and overweight differ by gender. The 1997-98 National Health Interview Survey (NHIS) found that men with incomes below the poverty level (57%) were somewhat less likely than men in the highest income group (64%) to be overweight (Schoenborn et al. 2002). However, women below the poverty level (57%) were considerably more likely to be overweight than women earning the highest incomes (38%).
Although children at all levels of society have grown heavier, those at the bottom of the socioeconomic scale have gained the most weight. Recent studies suggest that low socioeconomic status may be a risk factor for overweight among children as young as preschool age (Gerald et al. 1994; Sherman et al. 1995). The prevalence of overweight among 4-year-olds in the Supplemental Feeding Program for Women, Infants, and Children (WIC) was 10.6% (Mei et al. 1998), compared with 7.9% for a nationally representative sample of 4- to 5-year-olds (Ogden et al. 1997). Similarly, several studies of low-income preschool children attending Head Start programs found a high prevalence of overweight, ranging from 10% (Wiecha and Casey 1994) up to 32% (Hernandez et al. 1998).
Lower educational level is also associated with higher weight among both men and women, although the association is more striking for women. About six in 10 adults without a high school diploma were overweight compared to 52% of those with a graduate degree (Schoenborn et al. 2002). Similarly, some studies show an inverse relationship between weight and household income, and weight and parental education in children and adolescents, particularly among white children (Goodman 1999).
Influence of ethnicity
The 1997-98 NHIS (sample of 68,556 adults) found that black and Latino adults were twice as likely as Asian adults to be overweight (Schoenborn et al. 2002). Slightly more than one-half of white adults were overweight in the 1997-98 NHIS. The highest rates for childhood overweight were found in Latino and Native American children and black girls.
How do we distinguish between the influence of socioeconomic status and that of race or ethnicity? White children from lower income families experience a greater prevalence of overweight than those from higher income families (Troiano and Flegal 1998). However, family income does not reliably predict overweight prevalence in Mexican American and black children. An association between socioeconomic status and overweight has been found in white girls, but not in black girls (Patterson et al. 1997).
Nutrition and food insecurity
Women of low socioeconomic status are about 50% more likely to be obese than those at high incomes, while for men the obesity risk is similar regardless of income.
Overweight is generally associated with excessive food intake while food insecurity is associated with inadequate food supplies. How can both be found in the same individuals and households? Overweight is not just a function of the quantity of food consumed and can mask other nutritional problems that result when families have insufficient money for food. One possible scenario is that high-fat, high-sugar foods are the cheapest source of calories for low-income parents to buy. Reliance on these foods may contribute to weight gain, especially when it occurs cyclically in response to dwindling food dollars. Another scenario is that low-income parents may buy less high-fat, high-sugar foods when they are food insecure and then indulge in more when they have money.
Overweight and obesity are risk factors for:
-
Diabetes
-
Heart disease
-
Stroke
-
Hypertension
-
Gallbladder disease
-
High blood cholesterol
-
Complications of pregnancy; infertility
-
Menstrual irregularities
-
Increased surgical risk
-
Osteoarthritis (degeneration of cartilage and bone of joints)
-
Sleep apnea and other breathing problems
-
Some forms of cancer (uterine, breast, colorectal, kidney and gallbladder)
-
Stress incontinence (urine leakage caused by weak pelvic-floor muscles)
-
Psychological disorders such as depression
Glossary
Food security: Access by all people at all times to enough food for an active, healthy life. It includes at a minimum: (1) the ready availability of nutritionally adequate and safe food; and (2) an assured ability to acquire acceptable food in socially acceptable ways (such as without resorting to emergency food supplies, scavenging, stealing or other coping strategies).
Overweight and obesity: Regardless of gender, adults with a body mass index (BMI) between 25 and 30 are described as overweight, and with a BMI of 30 or more as obese. BMI is calculated by dividing weight (in kilograms) by height (in meters) squared. Children who are at or above the 95th percentile of BMI, using Centers for Disease Control (CDC) standards, are termed overweight. There is no one BMI cutoff for children because the number changes with age. Children at or above the 85th percentile are categorized as at risk for overweight. The term obesity is generally not used with children.
While these scenarios focus on individual behavior, another considers the genetics of obesity. In examining the relationship between food insecurity and overweight among the poor, recent studies have begun to look at the possibility that the body may make permanent changes in response to periodic food shortages, leading to increased body fat when food becomes available. For example, the thrifty genotype hypothesis of obesity suggests that those exposed to fluctuating calorie intakes develop adaptive methods to achieve high efficiency in energy use and deposition of fat stores (Neel 1962). The thrifty gene, which favors energy storage, may have been adaptive for early humans or traditional societies faced with periodic famine but is no longer beneficial in modern societies.
Yet another theory focuses on some evidence that low socioeconomic status leads to psychosocial stress, promoting increased fat deposition in the abdominal area through psychoneuroendocrinological pathways (Bjorntorp 1995). In spite of the many plausible theories, we still do not know all of the factors contributing to the obesity epidemic.
Overweight is not merely a function of the amount of food consumed; rather, it can indicate the challenging nutritional decisions that families must make when money is short. Left, UC Cooperative Extension offers nutrition education and food preparation classes.
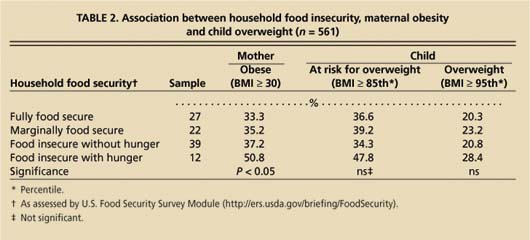
TABLE 2. Association between household food insecurity, maternal obesity and child overweight (n = 561)
Studies have found a relationship between overweight/obesity and food insecurity in adult women. Using a nationally representative sample of the U.S. population, women who were mildly and moderately food insecure (defined as having enough to eat but not always the preferred kinds of food) were more likely to be overweight than those who were food secure (Townsend et al. 2001). Controlling for other variables, these women were 30% more likely to be overweight in this study. Similarly, other studies with small sample sizes have found that the relationship between food insecurity and obesity found in women is not observed in men and young children. While it is not clear why this is so, it could potentially have something to do with the woman's role as caregiver, where she tries to protect the health of other family members through differential allocation of the scarce food resources.
In the UC study, obesity in U.S.-born Latino women was related to childhood experiences of food insecurity. Above, schools play an important role in teaching healthy eating habits.
Study of Latino mothers, children
The UCCE Body Weight and Health Workgroup convened seven advisors, four specialists and four other professionals to study the relationship between food insecurity and overweight in both women and children. A large group (n = 561) of low-income, mainly recent immigrant Latino mothers and their children aged 3 to 6 years, was selected for study. The families were recruited from four rural (San Benito, San Joaquin, Stanislaus, Tulare) and two urban (Contra Costa, Sacramento) California counties with high percentages of low-income Latino families. We hoped to answer four questions:
-
Is current household food insecurity related to overweight among the mothers?
-
Is a woman's childhood food insecurity related to her overweight as an adult?
-
Is current household food insecurity related to overweight status of her child?
-
Is a mother's past food insecurity related to her child's current weight status?
In 2001, our bilingual interviewers recruited mothers with the help of community-based agencies that serve food-insecure families, such as the WIC program, Head Start, migrant camps, health departments, health centers and family resource centers. To be eligible for participation, a mother needed to: (1) identify herself and her child as Mexican, Latino, Hispanic or similar; (2) have given birth to at least one child between June 1, 1995, and Feb. 1, 1998; (3) have a family income at or below 200% of the poverty level; (4) be at least 18 years old or an emancipated minor; and (5) sign a consent form. Mothers who were pregnant, planned to move in the next 2 weeks or had reported or perceived issues or illnesses that could influence accurate responses were excluded. We interviewed participants in private rooms in the health or WIC clinics, and in their homes if necessary. At the end of the interview, each participant received a gift certificate worth $20 at a local store.
We carefully measured the heights and weights of all mothers and children, and asked questions related to age, mother's education, household income, participation in food and monetary assistance programs, household size, language spoken at home, country of birth and years in the United States (table 1). Additionally, we used the 18-item U.S. Food Security Survey Module, formerly known as the Core Food Security Module, to collect data pertaining specifically to our four study questions and assess household food insecurity. Because that instrument only asks about food insecurity during the last 3 months, we added questions about food security during the past 12 months and during the mother's childhood. A food insecurity score was calculated based on the responses to these questions.
Widespread overweight and obesity
Of the low-income mothers in our study, 40% were overweight and 37% were obese. These numbers are similar to recent national figures for Mexican American women of all ages classifying 32% as overweight and 40% as obese (Flegal et al. 2002). Twenty-two percent of the children we studied were overweight, double the recent national prevalence of 11% for Mexican American 2- to 5-year-old children (Ogden et al. 2002).
We found that many of the women experiencing food insecurity were overweight (table 2). Approximately 60% of the women reported that their food situation was currently insecure. In our group of Latino mothers of young children, current food insecurity was directly related to overweight. As food insecurity increased, the likelihood that a mother was overweight also increased. We did not find a comparable relationship between current household food insecurity and overweight among the children.
Among some women, overweight was also related to the childhood experience of food insecurity. Seventy-eight percent of the women reported past experience of food insecurity in their own childhood. Interestingly, mothers who experienced severe levels of food insecurity as children were somewhat more likely to now be raising children who were overweight compared to other children in our study. In other words, the experience of food insecurity may influence the next generation to come.
Economics influences food habits
Why is food insecurity of these mothers related to overweight? There are monthly, seasonal and cyclical changes associated with variable incomes, changing food allowances and food availability, and other changing family and household circumstances. This variability may lead to eating patterns conducive to unhealthy weight gain. For example, during periods when funds are available for food purchases, there may be episodic binge-eating to compensate for times of deprivation. When food and money is available families may snack more and eat at fast-food restaurants. And during insecure periods, meal patterns may be altered and lower-priced, readily available foods with higher fat content may be consumed.
Role of food assistance programs
Some preliminary data indicates that participation in food assistance programs may improve food choices and reduce the prevalence of overweight. Nutrition education provided by the Expanded Food and Nutrition Education Program (EFNEP) and the Food Stamp Nutrition Education Program (FSNEP) teaches clients how to change their diets by shopping, preparing and serving more healthful foods to their families. In addition, a steady supply of food dollars (such as food stamps or WIC vouchers) can also allow families to make healthier choices (Mitchem 2003).
A study by the Centers for Disease Control and Prevention (1996) concluded that the WIC program for low-income children provides foods with essential nutrients without contributing to overweight.
Exposure to lifelong activities such as swimming, at this public pool in Parlier, above, as well as dancing, aerobics and running, can help children develop healthy exercise habits.
A crucial finding of our study was that obesity prevention requires that food selection, even in food insecure families, should be directed toward healthful choices. We also found that childhood circumstances may have a large impact on adult life and dietary preferences are often molded at a young age. Although household food insecurity was not related to overweight among the young children we studied (table 2), we do not know whether that relationship changes as the children mature. While longitudinal data must be collected to confirm our findings, we suspect that the effects of food insecurity may be carried across generations.
Healthy lifestyle choices
UCCE plays an integral role in addressing major health issues at the community level. This study laid the foundation for workshops targeting health professionals and policymakers in the six counties studied and for the development of education interventions targeting food-insecure, low-income Latino families.
Obesity is an extremely complex health issue influenced by many factors; successful interventions must include multiple approaches and partnerships. The Body Weight and Health Workgroup believes that a comprehensive approach must include policy changes in the food assistance programs, schools, food industry and the greater community. Implementation of these recommendations can empower community members to make healthy lifestyle choices.
Food assistance programs
In their capacity as direct service providers, food assistance programs can assist food banks and emergency food pantries to provide healthful food supplies; ensure that using food stamps is easy for shoppers, vendors and farmers; fund and promote programs linking low-income groups to healthy foods such as the WIC Farmers Market Nutrition Program; enhance food-stamp outreach to include the elderly and working poor; and ensure that nutrition education is available to all food-insecure families.
Food industry
The food industry should be encouraged to limit marketing targeting children; provide healthy food and beverage selections in school vending machines; and label fast foods to show fat, sugar, sodium and calories.
Schools
After family, schools provide the best opportunity for teaching healthy eating habits. They can teach basic food-preparation skills and the benefits of healthy eating and physical activity; provide longer physical education classes that promote lifelong activities such as dance, step aerobics, weight training and swimming; promote peer support groups or clubs where students can learn and practice skills in healthy eating and physical activity; sponsor physically active family events; and create an emotionally safe environment where everyone is encouraged to participate in physical education activities regardless of size and ability.
The workgroup recommends a comprehensive approach to addressing the epidemic of overweight, via partnerships with food assistance programs, schools, the food industry and community programs. For example, left to right, community programs such as gardens can help families get exercise while growing healthy food, and schools can show kids fun ways to be active and prepare healthy snacks.
Community groups
Community groups can advocate for safe, clean neighborhood areas conducive to physical activity and recreation, including sidewalks, crosswalks, bicycle and walking paths, parks and open spaces; physical education and nutrition in schools; and smaller portions and more healthful foods in restaurants.