Calag Archive
Calag Archive
Preventing obesity: What we eat?
Publication Information
California Agriculture 61(3):112-118. https://doi.org/10.3733/ca.v061n03p112
Published July 01, 2007
PDF | Citation | Permissions
NALT Keywords
Abstract
To curb the escalating rates of obesity in California and across the nation, it is imperative to identify dietary behaviors that prevent excessive weight gain. Reports in the press are often conflicting and more often confuse than clarify the issue of what people should eat to prevent obesity. We recently conducted a comprehensive review of the literature published between 1992 and 2003 on the dietary determinants of obesity in children and adults. We examined secular trend data, mechanistic research, observational studies and prevention trials. We found that the dietary factors related to increased obesity were high intakes of dietary fat, sweetened beverages and restaurant-prepared foods, and the increased likelihood of skipping breakfast. Factors most likely to protect against obesity were the higher consumption of dietary fiber, fruits and vegetables, calcium and dairy products.
Full text
The rapid rise in body weight of Americans has led top health officials to label obesity a national crisis. Since the 1970s, the prevalence of obesity has doubled among adults and tripled among children in the United States (CDC 2002). California is not exempt from this crisis. In 2001, more than 4.7 million Californians, or 19% of all adults, were obese (Lund et al. 2004). Obesity increases the risk of myriad health problems, including type 2 diabetes, cardiovascular disease, renal and liver disease, gastrointestinal disorders and certain forms of cancer. Managing obesity-related health problems is a major burden to the state and national health-care systems. The high costs and limited success of treating obesity that has already developed make prevention essential. However, efforts to design effective dietary interventions have been stymied by conflicting and inadequate understanding of the multiple causes of obesity.
An analysis of thousands of peer-reviewed obesity and nutrition studies published between 1992 and 2003 found that fruits and vegetables contribute to weight maintenance, because they are simultaneously low in calories and filling.
The rising rates of obesity are paralleled by a marked increase in the amount of research being conducted (fig. 1). However, the need for synthesis of research findings and the development of action recommendations is critical. The purpose of this article is to distill the research on key dietary factors that are crucial for inclusion in community nutrition-intervention programs designed to prevent obesity ( see page 124 ). These factors and the extensive supporting literature are drawn primarily from Woodward-Lopez et al. (2006) and Ritchie et al. (2005), and these references provide detailed methodology and background information on the studies that support the conclusions in this review. Although physical activity and sedentary behavior also play a role in the development of obesity, the focus of this review is on the role of dietary factors.
Analyzing the evidence
To understand emerging evidence on the dietary determinants of obesity, we recently completed a 3-year project to systematically review the scientific literature. This review was conducted under the guidance of the Obesity Prevention Network (OPN), convened by the Centers for Disease Control and Prevention. Reviewers with expertise in nutrition and/or obesity included researchers from seven universities and representatives from 12 state health departments across the country. Relevant studies published between 1992 and 2003 were identified from a search of the PubMed database, as well as from studies cited in other research papers and review articles. Specified search terms were utilized according to the topic of interest. For example, for the topic “sweetened beverages,” search terms included obesity, soda, soft drinks, sweetened beverages and fruit drinks.
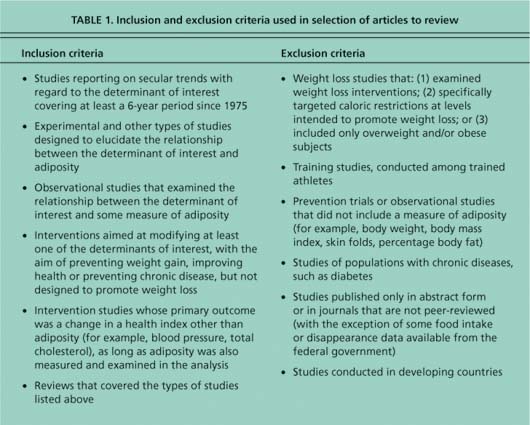
Specific inclusion and exclusion criteria were adhered to in the selection of articles to review (table 1). The focus was on studies of humans, both children and adults. Each selected article was abstracted on an article review table by an OPN member in order to systematically collect information about sample size and demographics, sampling strategy, study design and duration, statistical analysis, control variables, assessment of independent and dependent variables, and study findings, strengths and limitations.
Fig. 1. Scientific publications on obesity since 1975, based on PubMed search of English-language publications that included an abstract.
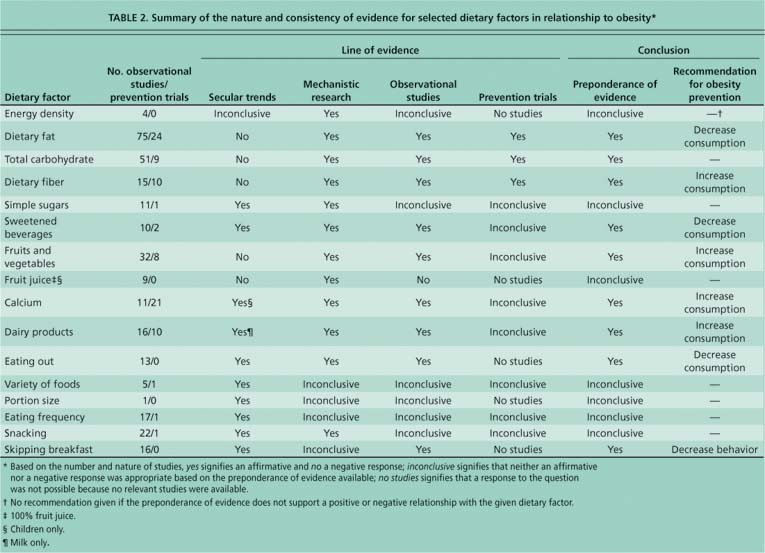
We examined four lines of evidence with respect to each dietary factor: (1) secular trends data, documenting changes in a determinant in the United States over the period that obesity has risen most steeply — since the mid-1970s; (2) mechanistic research that examined either a characteristic of a food, such as palatability or satiability, that is likely to affect energy intake; or experimental studies that examined how a diet-related factor might affect total energy intake; (3) observational studies in free-living (i.e., not in a laboratory setting) populations that examined the relationship between a diet-related factor and an outcome measure of adiposity, such as body mass index (BMI), body fat or waist circumference; and (4) prevention trials aimed at intervening with weight gain or the development of chronic disease that included a measure of adiposity but were not designed specifically to promote weight loss or treat obesity (table 2).
For each dietary topic, an evidence analysis group was formed of OPN members. For each line of evidence, the group addressed the number and merits of the studies reviewed and answered the question, “Does the preponderance of the examined evidence, based on strength and consistency, support that dietary factor X is a determinant of obesity?” For each line of evidence, this question was answered yes, no, inconclusive or no studies, based on specific criteria. A more detailed description of the methods and findings, including a discussion of the merits and limitations of the studies reviewed in arriving at conclusions, can be found in Woodward-Lopez et al. (2006).
What the evidence tells us
Energy density.
The consumption of excess energy — in relation to needs — leads to weight gain. Since the mid-1970s, per capita energy intake in the United States has substantially increased (Troiano et al. 2000; Putnam et al. 2002). Energy density, the number of calories in a given weight of food, is one metric that is used to distinguish between foods with higher and lower energy contents. Our current food supply abounds with energy-dense, nutrient-poor foods — typically highly processed foods that contain relatively large amounts of fat and/or sugar. Nearly one-third of the total energy intake among adults comes from these foods, and the more energy-dense the diet, the higher the total energy intake tends to be (Kant 2000).
Table 2. Summary of the nature and consistency of evidence for selected dietary factors in relationship to obesity*
However, at present it is not possible to conclude that manipulating the energy density of the diet would be an effective strategy for preventing obesity. This is because of assessment difficulties and the use of variable methods to calculate energy density (for example, the inclusion of all foods and beverages versus the inclusion of only energy-containing foods), and mixed findings (showing no relationship or a positive relationship) from the limited number of observational studies on energy density in relation to weight status.
Dietary fat.
A majority of the U.S. population consumes fat in excess of U.S. dietary recommendations for health; only about one in three Americans met the 2000 dietary guideline of less than 30% of calories from fat (Kennedy et al. 1999; Troiano et al. 2000). (As of 2005, the dietary guideline for fat was 20% to 35% of calories; previous editions of the dietary guideline recommended no more than 30% of calories from fat.) Mechanistic studies show that dietary fat, because of its high caloric content, palatability, and efficient utilization and storage, may be more problematic for weight maintenance than other macronutrients (Parsons et al. 1999). The preponderance of evidence from both observational studies and intervention trials further supports the conclusion that the consumption of high-fat foods is a risk factor for excessive weight gain.
Carbohydrate, fiber, sugar.
Carbohydrates are a heterogeneous group of food components ranging from simple sugars (such as sucrose and fructose) to complex carbohydrates (such as dietary fiber). Carbohydrates are not alike with respect to obesity risk. Although the intake of most types of carbohydrates, including dietary fiber, has risen concurrently with total food intake in recent years (Enns et al. 1997), the preponderance of evidence suggests that dietary fiber may be beneficial in abating obesity.
Carbohydrates in general, and dietary fiber in particular, are more satiating or filling and less energy-dense than dietary fats (Stubbs et al. 2000). Further, observational studies have consistently found that obesity is less prevalent with higher fiber intake.
Contrary to popular perception, the evidence on simple sugars, another form of carbohydrate, is more complicated and less conclusive than for dietary fat or fiber. Although experimental studies suggest that simple carbohydrates are readily overconsumed, in observational studies total sugar intake is either not associated with obesity or is negatively associated, meaning that thinner people tend to eat more simple sugars than fatter people. However, there is considerable evidence that some forms of sugar in the diet are indeed problematic.
Sweetened beverages.
Calorically sweetened beverages are a leading source of sugar in the typical American diet, and the con sumption of them has risen dramatically in recent decades (Jacobson 2001). Per capita consumption of soft drinks alone has increased from approximately 10 gallons per person in the 1940s to 60 gallons per person in the 1990s (Gerrior et al. 1998). Physiological compensation for energy consumed as a liquid appears to be less complete than when the same amount of energy is consumed as a solid food (Mattes 1996), so that consumption of sugar in beverage form is likely to result in higher total energy intake (Harnack et al. 1999). Also, fructose in the form of high-fructose corn syrup, which is commonly added as a sweetener in beverages, has emerged recently as a potential contributor to energy imbalance because of the way in which it is metabolized in the liver to favor lipogenesis. Fructose also fails to stimulate endocrine pathways that are known to regulate food intake and energy homeostasis (Havei 2001).
Substantial observational evidence also points to calorically sweetened beverages as a culprit in the obesity epidemic. In a study of school-aged children, each additional serving of a sweetened beverage consumed daily over a 1.5-year period increased the risk of becoming overweight by 60% (Ludwig et al. 2001). More recently, in a study published after our review, a 1-year, school-based intervention in the United Kingdom that decreased the consumption of soft drinks by only one-third-cup per day resulted in a 7% reduction in overweight compared to children in the control group (James et al. 2004).
Fruits and vegetables.
Fruits and vegetables may contribute to weight maintenance because of their low energy content and high satiety value. Although per capita vegetable and fruit intake has increased slightly since the 1970s (Putnam et al. 2002), only 41% of the population meets the recommendation for three to five daily servings of vegetables (GAO 2002). Further, more than one-third of what counts as vegetables in the U.S. food supply consists of iceberg lettuce, frozen potatoes (mostly French fries) and potato chips (Putnam et al. 2000). Observational evidence also supports that fruit and vegetable intake protects against obesity. The finding that fruits may be more protective than vegetables may be a function of how fruits and vegetables are typically consumed. The benefits of vegetables, for example, may not be attained if they are typically consumed with large amounts of fat added during frying or topped with high-fat dressings, sauces or condiments (Lin and Morrison 2002).
Fast foods are typically higher in calories and fat, while lacking essential nutrients. Current data indicates that eating out more often increases the risk of weight gain. Above, a food stand at the California State Fair in Sacramento.
Fruit juice.
Fruit juice was examined separately from total fruit intake because it is a source of liquid calories and fructose and, by the same mechanisms as proposed for calorically sweetened beverages, could presumably contribute to excess energy intake and storage. On a populationwide basis, however, the excessive consumption of fruit juice is not nearly as common as the excessive consumption of calorically sweetened beverages. On a daily basis, Americans consume the weight equivalent of roughly four times more carbonated soft drinks than all types of fruit juice combined. Fruit juice intake has not changed substantially since the 1970s, during which time obesity has risen most steeply (Putnam and Allshouse 1999). This fact, together with a preponderance of observational data showing no relation between fruit juice intake and obesity, supports the conclusion that fruit juice is not a critical behavior to target for obesity prevention. All of the observational studies that we examined on fruit juice intake in relation to obesity involved children only. However, because fruit juice intake tends to decrease as children get older, the excessive intake of fruit juice is an unlikely determinant of obesity in adults (Demory-Luce et al. 2004).
Calcium and dairy products.
Milk intake has decreased in recent decades, while the intake of cheese has increased. The mechanism whereby dairy intake might be related to weight has not been clearly established. There may be a biological effect on the energy balance of calcium or another component in dairy; an avoidance of dairy by overweight individuals concerned about additional weight gain; and/or a replacement of fluid milk with soft drinks and other calorie-containing beverages. There is some evidence that a high intake of calcium can influence energy balance by reducing adipose cell storage of fat and increasing fecal fat losses (Zemel et al. 2000). Other biologically active components in dairy may have additive effects. The preponderance of observational data supports the hypothesis that a low intake of dietary calcium and dairy is related to higher adiposity. Although the differential effects of low-fat and nonfat versus high-fat sources of dairy have not been well studied, the increased consumption of low-fat dairy products and calcium-rich foods is consistent with recommendations for the prevention of cardiovascular disease and the promotion of bone health.
Eating out.
Eating out is increasingly the norm. In the 1970s, U.S. households reported spending 20% of food dollars on foods eaten away from home. By the 1990s, that number had nearly doubled (Schwenk 1995). Patrons are often encouraged to purchase meals that contain more calories through “value” marketing or “super-sizing,” and restaurants are serving much larger portions. For example, in 1957 a typical hamburger from a fast-food restaurant weighed approximately 1 ounce, compared to up to 6 ounces in 1997. An 8-ounce soda typically served in 1957 now weighs in at 32 to 64 ounces (Nicklas et al. 2001). Further, fast food and restaurant foods are typically high in calories and fat, lacking in other essential nutrients, and highly palatable (Schwenk 1995; Jeffery and French 1998). Although additional studies are needed that use a standardized definition of fast food and eating out, the observational evidence to date suggests that the more one eats out, the harder it is to avoid weight gain.
Variety of foods.
Variety is defined as the inclusion of many foods in the diet that differ in one or more sensory qualities, such as color, taste or texture (Raynor and Epstein 2001). Eating a variety of foods has long been recommended as critical to achieving nutrient adequacy (Westenhoefer 2001), but it has also been implicated as one of the factors that encourage restaurant patrons to overeat. Short-term laboratory studies in humans indicate that increasing the variety of foods offered results in greater food, and consequently energy, intake (Jeffery and French 1998).
The variety of foods available in the United States has increased dramatically in recent years. In 1970, the number of new food products introduced into the marketplace was a little over 1,000; by 1996 that number had increased to over 13,000 (Gallo 1997). The majority of new food products are energy-dense, nutrient-poor foods like candy, snack foods and bakery items, rather than fruit and vegetable products (Young and Nestle 2002). However, most epidemiological studies of dietary variety have focused on the variety of healthful foods and have not examined influences on weight status. The scant few studies that compared variety of the diet to obesity in humans have had inconsistent findings, variously showing a positive, a negative or no relationship between dietary variety and adiposity.
Far left, Americans are snacking more than they did in the 1970s, and the snacks they eat tend to be higher in calories and fat than meals.
Taken together, the evidence available to date suggests that the influence of dietary variety on energy balance and adiposity depends on how variety is defined and the classification of foods being considered. We hypothesize that a promising strategy for weight management is to restrict the variety of energy-dense, nutrient-poor foods consumed and increase the variety of low-energy-dense foods, such as fruits and vegetables. However, this hypothesis merits further study before firm recommendations on variety of foods can be decisively adopted.
Portion size.
Americans report consuming increasingly large portion sizes of a majority of foods (Smiciklas-Wright et al. 2003). This trend has been found for foods such as salty snacks, desserts, soft drinks, fruit drinks, French fries, hamburgers, cheeseburgers and Mexican foods, whether consumed at a restaurant or at home (Nielsen and Popkin 2003). Short-term experimental trials in humans have shown that energy intake tends to increase with exposure to large portion sizes of most foods, but there are some notable exceptions (Rolls et al. 2000; Rolls et al. 2002). In one study, the energy intake of a meal increased after the consumption of a high-energy-dense salad, but decreased after consumption of the same-sized portion of a low-energy-dense salad (Rolls 2003). In this study, the energy density of the salad was manipulated by adding salad dressing and cheese. We hypothesize that there may be an interrelationship between portion size and energy density (the number of calories in a given weight of food), such that it is advisable to decrease the portion size of the most energy-dense foods and increase that of the least energy-dense foods. Unfortunately, the evidence associating portion sizes directly with overweight is limited at present, precluding a conclusive recommendation.
Eating frequency.
Paradoxically, small, frequent meals have been recommended both as a way to increase satiety and prevent weight gain, and as a way to overcome reduced appetite and limit unintentional weight loss. Total eating frequency has risen concurrently with the prevalence of overweight (Cutler et al. 2003). However, interpreting the evidence on eating frequency is complicated by the use of disparate definitions for what constitutes an eating episode. In some studies, only meals were counted, while others included both meals and snacks; what comprises meals versus snacks was not consistently classified across studies. Further, observational studies have had mixed results. A higher number of eating occasions has been associated with increased weight and decreased weight, as well as with no difference in weight compared to a less-frequent eating pattern.
Snacking.
The frequency of snacking by Americans has increased since the 1970s (ARS 2000). Snacks tend to be higher in energy density and fat content than meals (Jahns et al. 2001), and high snack consumption has been associated with an increased intake of fat, sugar and calories (McNutt et al. 1997). The preponderance of observational evidence suggests, however, that the frequency of snacking is not associated with obesity. We hypothesize that how frequently a person snacks may be less important than what and how much she or he eats when snacking, but there is presently not enough consistency in the findings to substantiate a decisive conclusion on snacking.
Skipping breakfast.
Population-based surveys have revealed that many people skip breakfast and eat more food later in the day, and that this pattern has increased since the 1970s (Raines et al. 1996; Siega-Riz et al. 1998). Observational studies fairly consistently have found that overweight individuals are more likely to skip breakfast or to eat a smaller breakfast than their leaner counterparts. Although there are few longitudinal studies that examine the relative influence of different types of breakfast (for example, whether having a doughnut for breakfast is better than eating no breakfast at all), the preponderance of evidence suggests that eating breakfast offers some advantage in preventing overweight.
What can be done?
Eating is a complex behavior. Foods vary widely, and those consumed are a result of many factors, including food purchasing and preparation, snacking and meal patterns, and other actions that affect dietary intake. Our approach of systematically examining and weighing numerous lines of evidence on the individual dietary determinants of obesity is consistent with this complexity. Restricting our review to one study type — most often randomized, controlled trials — eliminates the inherent difficulty involved in comparing studies of different designs and may allow the statistical analysis of findings from several studies to be combined (for example, meta-analyses). The approach used in this review, while more subjective, has the advantage of including a broader array of studies. Examining consistencies across different lines of evidence strengthens any conclusions derived from a single type of investigation.
Left, overweight persons are more likely to skip breakfast or to eat smaller breakfasts than normal-weight persons. In addition to skipping breakfast, research suggests that eating fatty foods, sweetened drinks, restaurant foods and prepared foods all contribute to excessive weight gain.
Based on our examination, no single dietary factor emerges as having an isolated influence on weight status, but rather a pattern of dietary intake appears important for the maintenance of energy balance. The dietary patterns identified as conducive to excessive weight gain include a high intake of dietary fat, sweetened beverages, restaurant foods and prepared foods, as well as skipping breakfast. Dietary factors that protect against excessive weight gain include the consumption of dietary fiber, fruits and vegetables, and calcium and dairy (table 2). Based on existing evidence, we found that the intake of dietary protein, simple sugars and fruit juice, as well as food variety, portion size, frequency of eating, and snacking were not consistently related to obesity. Studies of food variety and portion size in relation to overweight development were particularly limited.
The evidence from studies of children tended to be less conclusive than studies of adults, a finding that may reflect the difficulty in accurately measuring the typical consumption patterns of children, as well as the inherent fluctuations in energy balance that occur during growth. However, given that lifelong dietary habits are in large part established in childhood, and that adult overweight often begins in youth, it seemed most prudent and practicable to draw a single set of conclusions for all age groups, rather than differentiating between children and adults.
Several dietary factors emerged as priorities for future research, based on a promising but inadequate number of studies and/or being part of common dietary recommendations or practice, even though limited evidence currently supports a relationship with adiposity. Longitudinal studies and intervention trials relevant to public health efforts in California were particularly lacking, including studies of the Latino population.
Although researchers continue to gather evidence on obesity prevention, concerned public health agencies and individual practitioners cannot wait to take action. Current evidence suggests that practitioners should encourage breakfast consumption and increased intakes of fruits, vegetables and low-fat dairy foods, along with the decreased consumption of energy-dense, low-nutrient foods. Programs that address these dietary practices, along with promoting physical activity and reducing sedentary behaviors, are most likely to be effective in preventing obesity.