Calag Archive
Calag Archive
Seniors, and their food handlers and caregivers, need food safety and nutrition education
Publication Information
California Agriculture 68(1):30-37. https://doi.org/10.3733/ca.v068n01p30
Published online January 01, 2014
NALT Keywords
Abstract
Seniors are at greater risk than other adults for foodborne illness, poor nutrition and high rates of nutrition- and lifestyle-related chronic diseases. They also represent a major underserved segment of the UC Cooperative Extension client population. The Make Food Safe for Seniors (MFSFS) initiative assessed food safety and nutrition education needs of fixed-income seniors and food handlers and caregivers serving seniors in 10 California counties. Baseline survey results found unsafe practices by over 50% of the participants in six areas — and by over 65% of participants in three of those areas. After one food safety training, a post-test showed an average knowledge gain of 18.1%; seniors had gained the least knowledge, food handlers had gained some knowledge, and caregivers had gained the most. The unsafe food handling practices of a majority of the study group, as well as poor food behaviors, suggested areas in which education could reinforce or improve food safety, healthy eating and disease prevention practices of seniors, caregivers and food handlers serving seniors.
Full text
The coming of age of baby boomers accelerated the rate at which California's population is turning gray. In “The Graying of California,” a special issue of this journal, UC Division of Agriculture and Natural Resources (UC ANR 2010) acknowledged this as an emerging concern. Public health professionals for many years have been concerned that the workforce is not adequately prepared for the needs of America's aging population (Krisberg 2005). In our research we were concerned about the rapidly increasing numbers of older Californians at greater risk for food-borne illness (food poisoning) as well as their need for nutrition education to promote healthy aging (Blackburn 2010).
In a study of the food safety and nutrition practices of senior citizens and their food handlers and caregivers, UC Cooperative Extension researchers identified a need for food safety and nutrition curricula aimed at seniors and those who prepare their food. Above, participants at a food safety training in Alameda County learn how to calibrate a food thermometer.
Risk of foodborne illness
Adults over the age of 60 are more likely than younger adults to experience complications, hospitalization and death because of foodborne infections (Cates et al. 2009). Seniors with diminished capacity or physical impairment — who are taking multiple medicines or have weakened immune systems — are less able to fight foodborne pathogens, such as Salmonella, Escherichia coli O157:H7 and Listeria, and other bacterial or viral infections (Kendall et al. 2006).
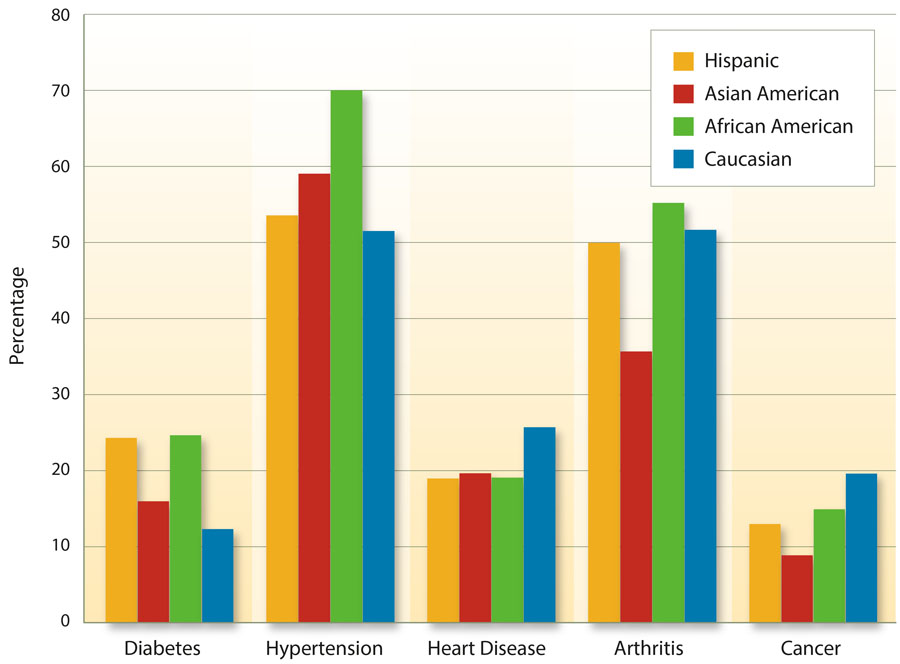
About 80% of seniors in the United States have at least one chronic health condition, and 50% have at least two; some chronic conditions render them more susceptible to foodborne illness (CDC 2011a). About 3.6 million Californians are over age 65. At least 55% of these seniors suffer from hypertension, 50% from arthritis, 24.0% from heart disease, 17.3% are diagnosed with cancer and 14.8% have diabetes. These top five chronic disease conditions vary significantly in California by ethnic group (Wallace et al. 2003) (fig. 1).
Of major concern are those seniors who are suffering from deficits in memory functioning. Lapses in episodic memory (the recollection of personally experienced events) are an important contributing factor to unsafe food handling, missed or mistakenly repeated doses of medications and other high-risk behaviors (Ober 2010). This memory impairment is the hallmark of Alzheimer's disease, which occurs in 14.7% of 85-year-olds and 4.2% of 75-year-olds (Brookmeyer et al. 2007).
Safe food handling knowledge and skills are critical for seniors so they can recognize unsafe practices that may be used by untrained food handlers in community-based organizations or by untrained agency or kinship caregivers who lack knowledge of safe food handling. Many who provide food to seniors in need of assistance may not be aware that elderly populations are more vulnerable to foodborne illness. The population of seniors receiving care is significant:
California's In-home Supportive Services's case load in June 2012 was 432,650 people (CAPA IHSS 2012).
Low availability of food, insufficient resources and hunger may also contribute to the risks of foodborne illness among seniors. Hoarding food is a natural response in times of limited food supply, and unsafe food items may not be discarded. Concerns about finances among limited-and fixed-income elders in the current economic environment may be escalating: poverty estimates indicate that 810,000 of 4.3 million older Californians live in poverty (Bohn et al. 2013), and many fixed-income seniors live on an income that is 50% or less of the benchmark income for poverty in the United States.
Causes of foodborne illness
Primary factors contributing to food-borne illness are improper temperature, inadequate cooking, contaminated utensils or equipment, eating food from unsafe sources and poor personal hygiene. Research shows that elders who take food home from group sites or have home-delivered meals may fail to properly store or reheat the food. A study of the average wait time between when prepared meals are home delivered and when they are consumed found 63% of seniors ate their meals when delivered, 29% stored them in the refrigerator or freezer and 8% left them out. About 35% reported leftovers, but only 12% ate the leftovers within 2 hours as recommended (Almanza et al. 2007).
Foodborne illness in California
In 2011, the Centers for Disease Control (CDC) estimated that annually one in six Americans, or 48 million people, experience a foodborne illness; 128,000 are hospitalized, and 3,000 die (CDC 2011b). An earlier report combining data from multiple surveillance systems and sources estimated foodborne diseases cause approximately 76 million illnesses, 325,000 hospitalizations and 5,000 deaths in the United States annually (Mead et al. 1999). A recent study using the CDC model to determine cost, and adding consideration for pain suffering and functional disability, estimates an annual cost for foodborne illness of $77.7 billion (Scharff 2012). Increased rates of food-borne illness are associated with eating more food away from home, emerging food-borne pathogens, and a growing aging population more susceptible to foodborne illness.
The Centers for Disease Control Food Net Report (CDC 2011c) found a significantly higher incidence of at least five pathogens (Campylobacter, Listeria, Salmonella, Shigella and Vibrio) in California compared to a 10-state average. Cases of Campylobacter in California were 32.50 per 100,000 compared to the 10-state average of 13.52 cases (CDC 2011c). A 10-year review of California outbreaks from 1998 to 2007 found restaurants and other food establishments to be the most common locations for outbreaks (44%), followed by private homes (21%), multiple locations or unknown (8%) and the workplace (7%) (CSPI 2011). California Department of Health Services reported about 26% of foodborne illness is associated with food prepared in community locations such as potlucks or church dinners, 46% with restaurants, 19% with in-home preparation and 6% in schools (Wang 2000).
Another assessment of home-delivered meals (n = 179) found 58% of mostly older (age 80 and above) seniors stored all or some of the food. Of the older seniors who saved their food, 38% stored it in the refrigerator, but 30% stored it on the counter (Fey-Yensan et al. 2001). A study of 120 senior meal recipients, mostly females over age 70, found about 64% knew the importance of hand-washing but were not aware of when and how to wash hands (Lee et al. 2009). Lee and colleagues also found that home-delivered meal recipients (n = 97) had an average score of 63.8% in food handling, but 49% for cleaning, sanitizing and washing dishcloths.
A national representative Web-based survey (n = 2,060) examined refrigerator temperatures, use of thermometers and frequency of cleaning home refrigerators. About one half of all participants in the study had cleaned their refrigerator in the last month, but only 11% had a thermometer in their refrigerator (Kosa et al. 2007). More of the older adults (77.5%) were likely to have their refrigerator at the right temperature than the younger population (70.4%). However, older adults who were unmarried or lived alone were less likely to have a thermometer or have their refrigerator at the recommended temperature (40°F or below). More recent research shows an increasing trend in consumer food thermometer ownership from 49% in 1998 to 70% in 2010. The study found the elderly, 65 to 101 years old, were less likely to use a food thermometer for roasts and chicken parts than adults 18 to 29 years old (Lando and Chen 2012).
Make Food Safe for Seniors (MFSFS)
The Make Food Safe for Seniors (MFSFS) initiative is a joint research venture, funded by a CORE issues grant, between two UC ANR workgroups — Aging Californians in Rural and Urban Settings, and Food Safety. The research team was comprised of two Agriculture Extension Station scientists focusing on aging; a Cooperative Extension food safety specialist; nine Nutrition, Family and Consumer Sciences (NFCS) advisors; and county directors and community collaborators in 10 counties.
The objectives of the MFSFS initiative were to a) determine the baseline nutrition education and food safety needs of limited- or fixed-income seniors, food handlers in senior services and in-home caregivers, b) increase the food safety knowledge and skills of the study group, c) increase public awareness of the higher risk of foodborne illness among elders, d) use the findings to create senior-friendly curricula and materials to help reduce the risk of foodborne illness and e) promote healthy food practices for vulnerable elders in local California counties.
Local needs assessments.
The MFSFS team reviewed existing research and assessments of nutrition and food safety needs in local counties. Research by Barrett et al. (2005) with in-home caregiver trainees (n = 482) in Sacramento and Yolo Counties documented a dire need for standardized nutrition education and safe food handling curricula for caregivers working with frail elders aging in place. The 2009 California Health Interview Survey health risk data for baby boomers (both informal caregivers [n = 5,688] and noncaregivers [n = 12,941]) show that those who are also caregivers have greater odds of overall negative health behaviors associated with disability and chronic illnesses (Hoffman et al. 2012).
Blackburn (2010) assessed the nutrition and wellness needs of limited-income seniors at 20 sites (n = 377) in Alameda County. About 40% of the seniors reported multiple chronic diseases, and approximately 88% expressed a need for more healthy nutrition, lifestyle and food safety information, for example on cooking, preventing spoilage, and storing food over extended periods.
A 2005 Aging Californians workgroup survey of 27 NFCS advisors and county directors found few counties offered senior programs, but 86% said aging programs were needed in their counties (2005 Aging Workgroup, unpublished data).
Process.
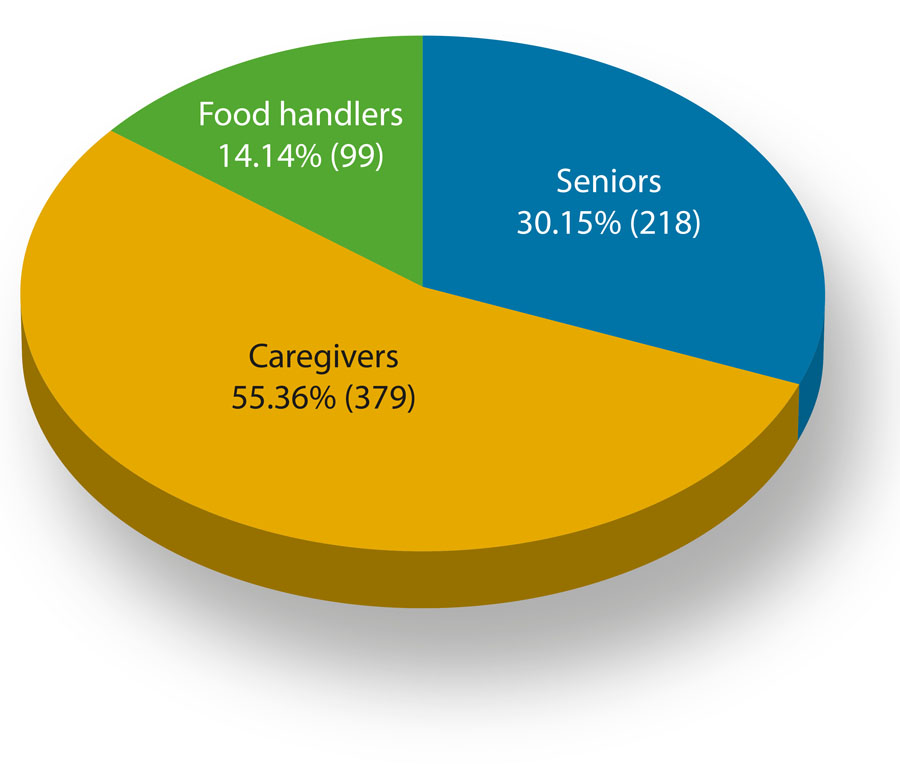
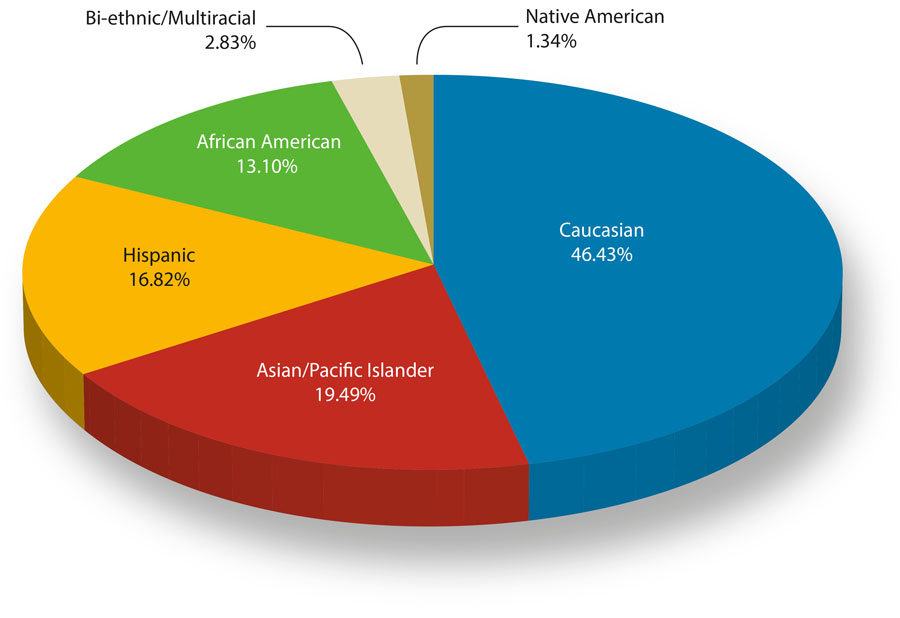
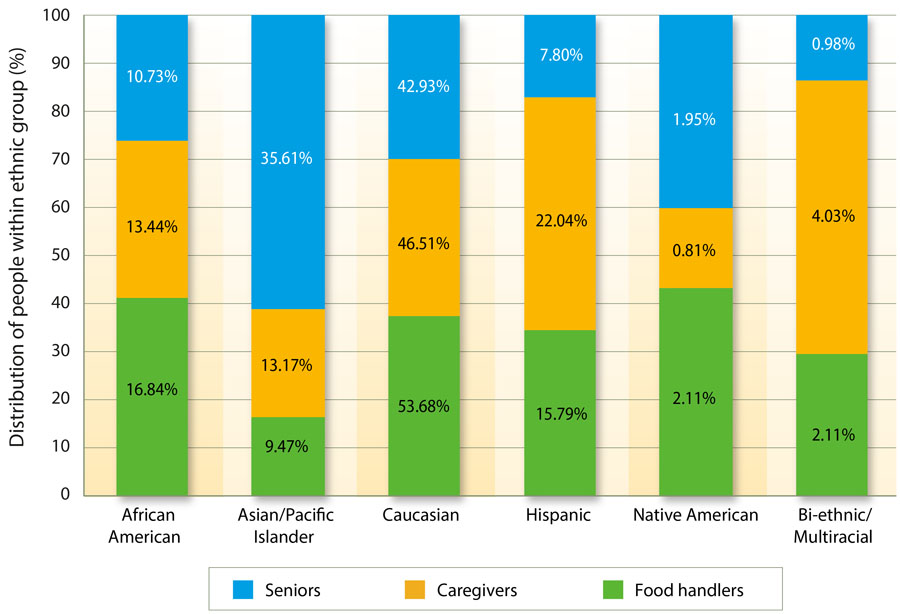
Our research protocol and evaluation tools were approved by UC Davis Office of Research Institution Review Board. An existing UC-approved food safety curriculum was adapted to reflect the needs and circumstances of the elderly and to effectively teach knowledge and skills to seniors, food handlers in senior programs and in-home caregivers. Cooperative Extension educators assessed and trained 696 participants from 10 counties (379 caregivers, 218 seniors and 99 food handlers) (fig. 2). Participants were from senior centers, senior food programs, in-home supportive services, and kinship caregivers. Ethnic composition of the study group was diverse (fig. 3), and the representation of seniors, food handlers and caregivers within each ethnic group is shown in figure 4.
Fig. 2. Study group was composed of 696 participants, including seniors who volunteered from senior centers and senior programs, caregivers from in-home supportive services and family or relative caregivers, and food handlers from church communities and food pantries.
Fig. 3. Study participants by ethnic distribution. Total number of participants who provided ethnic information was 672.
Fig. 4. Ethnicity of the seniors, caregivers and food handlers (read each color across the figure); and within each ethnic group, the percentage who were seniors, caregivers and food handlers (read the size of each color unit against the vertical axis).
Data collection.
Baseline data were collected between January 2008 and March 2009 with an 11-question pre-test of food safety knowledge and practices; the same questions were asked in the post-test later. Participants (n = 696) received 2 to 3 hours of interactive education in groups ranging in size from 10 to 22 participants. The education included information on the incidence of foodborne illness, which groups are at greater risk, causes and sources of foodborne illness, as well as the four basic components of food safety: cleanliness (personal hygiene, hand-washing and washing foods); proper cooking and chilling temperatures; keeping food at the right temperature and use of thermometers; and storing food to prevent cross contamination of raw and cooked meat or contamination by chemicals or objects.
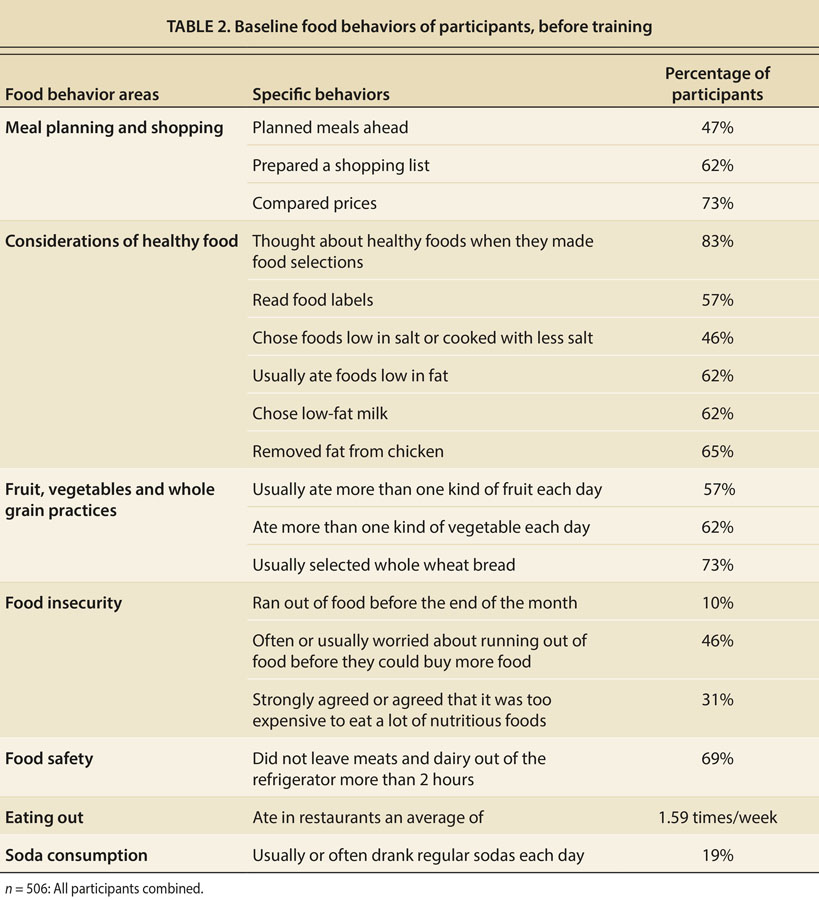
Baseline food behavior data also were collected before the food safety education with a USDA-approved food behavior checklist that was filled out by 506 of the 696 study participants. The checklist contains 21 questions about meal planning, food buying, food safety practices, healthy food choices, food preparation practices, reducing salt and fat intakes, eating fruits, vegetables and whole wheat bread, food availability and food security, eating out, and eating breakfast.
Data analysis.
The change in food safety knowledge as a result of the training was derived by comparing the pre-test and post-test scores of correct responses for individuals and the overall group. The P value for knowledge gain was derived by determining the probabilities of getting all answers correct for all the choices in the 11-question test. The pre-test null hypothesis — that is, the array of pre-test probabilities for correct answers — was determined by this formula:
If n = number of choices and c = number correct, then
To construct a null hypothesis for the post-test, one must account for the effects of the training intervention. In this study, it meant reducing the number of choices by counting each correct answer as “1”, which was selected because a larger integer eliminates choice for questions with just 2 possible correct answers. When choices are reduced by 1, the null hypothesis for each question (probability of correct answers by chance) increased by a certain percentage.
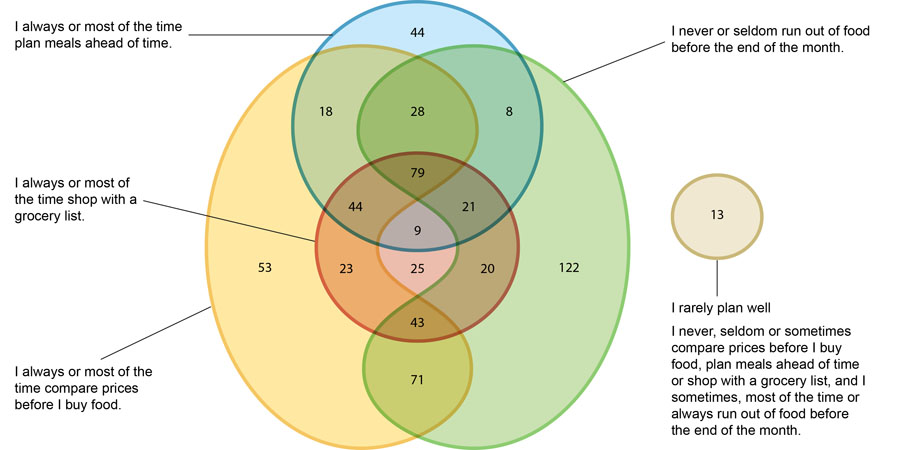
Baseline food behavior practices, from the food behavior checklist assessment, were entered into an Excel database, summarized, normalized and examined to determine the baseline nutrition education needs of the participants. Results from different questions were grouped into acceptable behavior targets toward achieving larger nutrition goals such as reducing fat, salt and sugar in the diet.
Baseline/pre-test results
Baseline food safety test results, before the training, show a serious need for basic food safety knowledge to help prevent foodborne illness among at-risk seniors. Many participants lacked correct information about cooking and cooling temperatures. For example, only 57% believed using a thermometer was the most accurate way to determine if foods are adequately cooked.
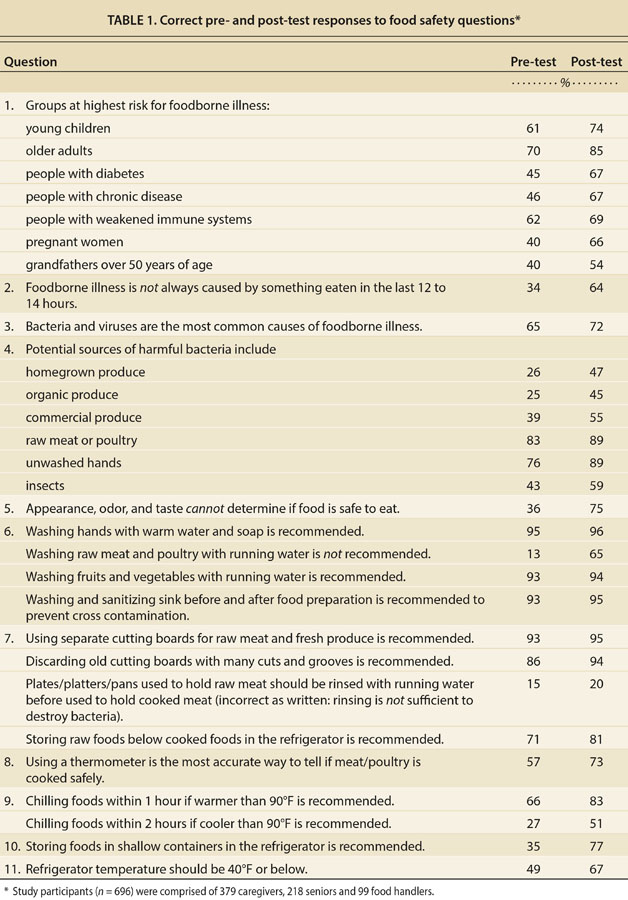
Pre-test data show more than 50% of the study group participants answered incorrectly six of the 11 food safety questions: 66% provided an incorrect response to the statement that “foodborne illness is not always caused by something eaten in the last 12 to 14 hours”; 64% believed, incorrectly, that appearance, odor and taste can determine if food is safe to eat; 65% did not know that food should be stored in shallow containers; 73% reported incorrect answers about chilling food when the temperature is less than 90°F and 34% when the temperature is over 90°F; 43% did not know that using a thermometer is the most accurate way to determine if food is accurately cooked; and 51% incorrectly identified the recommended refrigerator temperature. Also, many participants did not recognize the population groups at increased risk for foodborne illness: 70% identified older people as a group at risk but only 40% identified grandfathers; 40% knew that pregnant women are at risk; 45% identified diabetics as at risk; 46% knew people with chronic diseases are at risk; and 62% recognized people with weakened immune systems as being a vulnerable group for foodborne illness (table 1).
Knowledge gain/post-test results
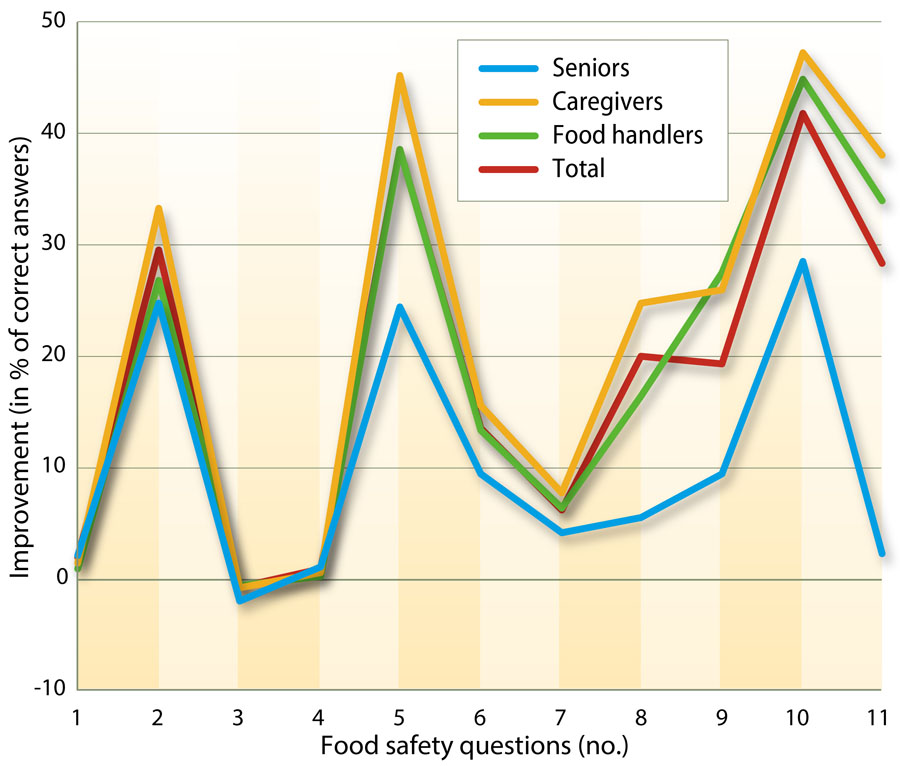
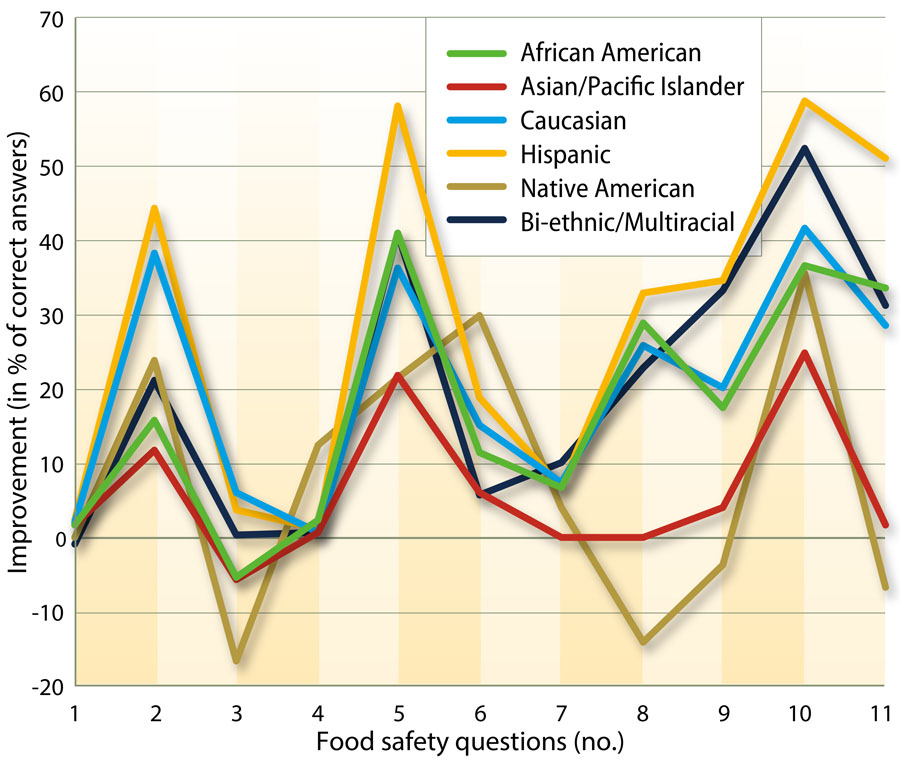
To assess the rate of knowledge gained from pre-test to post-test, a null hypothesis was derived that represented the difference between post-test and pre-test probabilities for correct answers. We used a chi-squared test to compare the actual knowledge gain to the expected (null hypothesis) knowledge gain. The comparison produced a probability (P value) that was at least as extreme as the null hypothesis (cut-off 0.05). Evaluation of the total group (n = 696) found an average increase in the percentage of correct responses from 58.0% to 76.1%, a knowledge gain of 18.1% (P = 0.4930). The gains of seniors (10.4%, P = 0.0404) were much lower than those of the in-home caregivers (23.4%, P = 0.9045) and food handlers (18.1%, P = 0.7195) as shown in figure 5. By ethnicity, P values for knowledge gain were Native American P = 0.9966, Hispanic P = 0.9960, Caucasian P = 0.7681, Bi-ethnic/Multiracial P = 0.6846, African American P = 0.6060, and Asian/Pacific Islander P = 0.0031 (fig. 6). The size of the Native American and Bi-ethnic/Multiracial groups were comparatively small, 9 and 19 participants, respectively, but all ethnic groups had significant gains in knowledge at different rates except for Asian/Pacific Islander (P = 0.0031).
Fig. 5. Knowledge gained from pre-test to post-test. Study group was comprised of 218 seniors, 379 caregivers and 99 food handlers (from church communities and food pantries). A chi-squared test was used to compare the actual knowledge gain to the expected knowledge gain.
Baseline food/nutrition behaviors
Table 2 summarizes the baseline food behaviors of the 506 study participants who completed the food behavior checklist. Of significance are the questions about food insecurity — 46% often worried about running out of food, 10% reported that they actually ran out and 31% felt it was too expensive to eat a lot of nutritious food. The research team grouped a series of baseline healthy behaviors into target goals under the areas listed in table 2. The performance of the group in relation to these goals was determined by Boolean analyses to detect deterministic dependencies between observed response patterns. Baseline performances of the study group to meal planning and shopping target goals are displayed in figure 7.
Fig. 7. Learning targets for good meal planning and shopping behavior goals, and the number of participants in the study group (n = 621) achieving them: 2.09% of the participants achieved no target (rarely plan well); 39.29% achieved one; 23.99% two; 21.90% three; and 12.72% all four targets.
Training needs, considerations
In the food safety knowledge pre-test, the MFSFS research team found food safety practices similar to the findings of a national representative survey (n = 1,140); older adults think they are knowledgeable about food safety but do not follow recommended food safety practices (Cates et al. 2009). Dutram et al. (2002) reported food safety education improved safe food-handling practices among low-income elders participating in congregate meal programs and home-delivered meal programs. The MFSFS post-test results point to a similar conclusion. The national study of older people by Cates et al. (2009) suggested men in particular and individuals with high income or education levels also need food safety education.
The positive findings in the MFSFS study were that in the pre-test 66% knew cooked food should be refrigerated within 1 hour if the temperature is over 90°F, and 67% knew the correct refrigerator temperature at post-test. Of most concern was the lack of knowledge about cross contamination of raw and cooked meat, potential sources of harmful bacteria, proper use of a thermometer to accurately determine if food is adequately cooked (some used taste, smell and appearance to determine if food is safe) and the increased risk with age for foodborne illness. By groupings, seniors knew relatively less than the food handlers or caregivers.
At a food safety training in Davis, Calif., participants used a GlitterBug UVA lamp to find out how thoroughly they washed their hands.
The research study was limited to a convenient sample of 696 people. Therefore, the results are not derived from a population-based sample, but they may point to the need for food safety as well as nutrition education among participants in UC Cooperative Extension's Nutrition, Family and Consumer Sciences programs.
Key to the effectiveness of food safety education among elders is the method of information delivery. Kosa et al. (2011), in a randomized control evaluation of the effectiveness of Web-based and print materials with older adults, found no significant differences between the two delivery methods. They suggested focusing education on a limited number of practices and combining print materials with personal contacts.
The MFSFS training used a client-centered, senior-friendly, interactive and hands-on educational approach, which achieved an average knowledge gain of 18.1%. Interactive education has been used very successfully in the Alameda County Quality of Life education program since 1993, and most recently in the 2012 Staying Healthy nutrition education program, completed by over 260 senior-housing residents with a graduation rate higher than 95%.
The research findings suggested the levels of knowledge retention differed among the three groups (seniors, food handlers, caregivers). The caregivers (some were much younger than the seniors) as well as the food handlers may have had some or more exposure to food safety information than the seniors. Research shows that older adults with prior knowledge of health information can retain it at levels that resemble those of young adults (Miller et al. 2013). Other research shows that with age, certain normal changes occur with the loss of episodic memory that might impact comprehension and knowledge retention (Ober 2010).
For older adults with low knowledge and those with low literacy, training must be tailored to fit individual learning needs (Miller 2010).
Potential for new curriculum
A 2008 statewide meeting of the ANR Umbrella Nutrition Workgroup voted a caregiver curriculum and training program to be a priority, and the 2010 special issue in California Agriculture on aging stated the need to assess the unique nutrition and wellness needs of aging Californians (Blackburn et al. 2010). Our research supports the need for training older adults and those who prepare their food to address food safety needs in the home and community. The training must seek to increase a) declarative and procedural knowledge surrounding food safety standards and b) skills surrounding how to apply those standards to ensure safe food preparation and storage. Importantly, the training also must be tailored to those most at risk for foodborne illness.
The data collected by the research team, described here, provides a knowledge base that could be used for Cooperative Extension nutrition and food safety curricula for seniors and caregivers in California and also to heighten awareness of the food safety needs of California's elders. The researchers have distributed this information through UC Delivers, a UC ANR website ( http://ucanr.edu/delivers/ ), and through conference presentations, peer-reviewed publications, national award applications, and educational interventions with providers and seniors in some counties. An outreach strategy is needed to disseminate the learning and the need for senior-friendly food safety and nutrition information statewide and nationally. In the long term, the MFSFS data and lessons learned could be used to develop a comprehensive UCCE nutrition, wellness and food safety curriculum for at-risk seniors and caregivers in California.