- Author: Kathy Keatley Garvey
Of the more than 30 million cases of COVID-19 in the United States, 547,000 people have died. They are not numbers: they represent family, friends, co-workers, colleagues, neighbors and acquaintances who have succumbed to this tragic disease.
And today Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention (CDC) warns of another surge. Our nation, she says, shows a seven-day average of about 57,000 new COVID-19 cases per day, a 7 percent increase over the last week.
A burning question: Why do some COVID-19 patients recover and some don't?
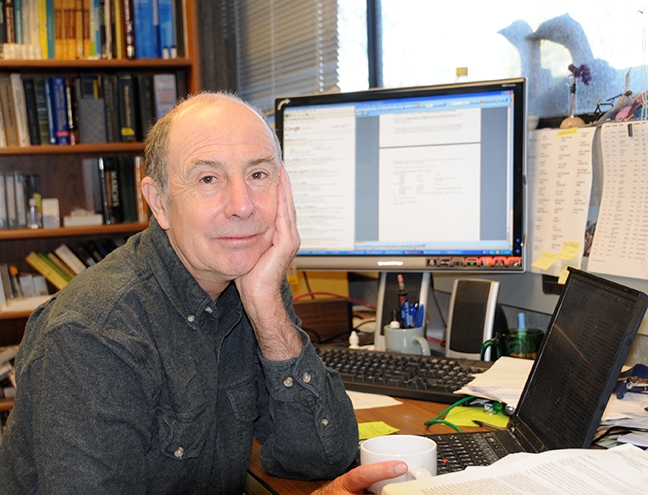
The laboratory of UC Davis distinguished professor Bruce Hammock, who holds joint appointments with the Department of Entomology and the UC Davis Comprehensive Cancer Center, may have just pinpointed why.

The team of eight UC researchers, primarily from the Hammock lab, found that four compounds in the blood of COVID-19 patients are highly associated with the disease. Their paper, “Plasma Linoleate Diols Are Potential Biomarkers for Severe COVID-19 Infections,” is published as open access in the current edition of Frontiers in Physiology.
ARDS, characterized by fluid build-up in the lungs, is the second leading cause of death in COVID-19 patients, next to viral pneumonia, according to the National Center for Biotechnology Information.
“Different outcomes from COVID-19 infections are both terrifying from a human health perspective and fascinating from a research perspective,” said UC Davis lead author and doctoral candidate Cindy McReynolds of the Hammock lab. “Our data provide an important clue to help determine what impacts the severity of COVID-19 outcomes. Initially, we focused on the immune response and cytokine profile as important drivers in severity, but considering what we now know from our study and others in the field, lipid mediators may be the missing link to answering questions such as why some people are asymptomatic while others die, or why some disease resolves quickly while others suffer from long-haul COVID.”
“The hypothesis advanced in this paper is that because the leukotoxins have been associated with serious illness and death in humans and dogs and the symptoms are those of adult respiratory distress syndrome, these compounds are biomarkers of pulmonary involvement in COVID-19,” Hammock said. “We also think that it is the conversion of leukotoxin to the toxic leukotoxin diol that causes pulmonary and perivascular edema and this could be leading to the respiratory complications.”
“So the leukotoxins and leukotoxin diols,” Hammock said, “are indicators of respiratory problems in COVID-19 patients as plasma biomarkers. They also present a pathway for reducing ARDS in COVID-19 if we could inhibit the soluble epoxide hydrolase, a key regulatory enzyme involved in the metabolism of immune resolving fatty acids.”
The UC Davis scientists used clinical data collected from six patients with laboratory-confirmed SARS-CoV-2 infection and admitted to the UC Davis Medical Center, Sacramento, and 44 healthy samples carefully chosen from the healthy control arm of a recently completed clinical study.
The Hammock lab's 50-year research on soluble epoxide hydrolase (sEH) and its inhibitors led the professor to found and direct EicOsis Human Health, a Davis-based company that is developing a potent soluble epoxide hydrolase inhibitor for pain relief. Epoxy fatty acids control blood pressure, fibrosis, immunity, tissue growth, depression, pain, inflammation and other processes.
But more recently, the Hammock lab has turned its attention to using sEH as a means to resolve inflammation associated with COVID-19 and the fibrosis that can follow.
The paper is the work of Hammock, McReynolds and Jun Yang (corresponding author) of the Department of Entomology and Nematology and EicOsis Human Health; Irene Cortes-Puch of the Department of Entomology and Nematology, EicOsis Human Health, and the Department of Internal Medicine's Division of Pulmonary Critical Care and Sleep Medicine; Resmi Ravindran and Imran Khan of the Department of Pathology and Laboratory Medicine; Bruce G. Hammock of UC Davis Department of Veterinary Medicine, Aquatic Health; and Pei-an Betty Shih of the UC San Diego Department of Psychiatry.
See the news story on the Department of Entomology and Nematology website at https://bit.ly/3lSWbwf
- Author: Kathy Keatley Garvey
That's Bruce Hammock, distinguished professor in the UC Davis Department of Entomology and Nematology who holds a joint appointment with the UC Davis Comprehensive Cancer Center.
In research published in the Proceedings of the National Academy of Sciences, the interdisciplinary team of scientists from the University of Pittsburgh School of Medicine, UC Davis, Geisel School of Medicine at Dartmouth, and Harvard Medical School linked a newly discovered class of bacterial enzymes to battling cystic fibrosis.
In analyzing secretions drawn from the lungs of cystic fibrosis patients at the Children's Hospital of Pittsburgh, the scientists discovered that the bacterium perpetuates inflammation by secreting an enzyme called Cif that sabotages the body's ability to make a key molecule called a "pro-resolving lipid mediator" and stop the inflammatory response it started.
The scientific discovery could lead to new therapies that would interrupt or correct the bacterial sabotage, Hammock and Bomberger said.
“This paper is the outcome of an exciting and interdisciplinary project,” said Hammock, who directs the UC Davis Superfund Program financed by the National Institutes of Health's National Institute of Environmental Health Sciences (NIH-NIEHS). “It started several years ago with the NIEHS Superfund Program funding both a group at Dartmouth and at UC Davis. A very productive and exciting collaboration resulted in looking at how to mitigate the effects of environmental chemicals on human health. Our collaborative work led to this joint publication which yields exciting hope for cystic fibrosis patients.”
Co-authors of the newly published research include two UC Davis researchers from the Hammock lab, Christophe Morisseau and Jun Yang.
Meanwhile, Bomberger continues to work on the biology of the system while the Dartmouth and Davis groups have developed inhibitors of the action of CIF to stabilize pro-resolving mediators, reduce inflammation, and control periodic flare ups of bacterial infections.
"It will be key to devise a way to remove P. aeruginosa's ability to capitalize on the body's natural inflammatory response, without eliminating that response," said Bomberger. "Inflammation is happening for a reason—to clear infection. We just need it to temper the response when it is not effectively doing its job or is no longer needed."
“We think that this research will lead to a very positive outcome to improve the lives of cystic fibrosis patients,” Hammock said. Some 30,000 Americans have cystic fibrosis.